Mammograms
The mammogram controversy is due to multiple competing issues: The desire to test and diagnose early, the excessive insults to the tissues from testing and surgical probing and the potential benefits overall. Lets look at the facts:
Mammograms benefit by detecting breast cancer at an early stage! The data clearly shows that 60-70% of all breast cancers are detected at DCIS or Stage I level. This imparts a significant survival advantage. However and there is a however in every story. The following “however” is a representation of all the known and validated information.
Mammograms below 40 years of Age:
Mammograms in younger women age less than 40 years have higher “false positives,’ and therefore are subjected to un-needed needle biopsies and further diagnostic radiation exposures for confirmation and re-testing. The NCI projects this false positive reading at 20% (2 in 10). This anomalous reading is primarily due to the increased breast density as a result of the milk ducts and fat ratio. But here in lies the additional dilemma whereby dense breasts are subject to a higher risk of malignancy and scrutiny.
("In a theoretical population of 10,000 women aged 35 to 39 years, 1,266 women who are screened will receive further workup, with 16 cancers detected and 1,250 women receiving a false-positive result.") (The researchers examined the medical records of more than 117,000 U.S. women who got their first mammograms between the ages of 18 and 39. In the ensuing year, not a single woman under the age of 25 was diagnosed with breast cancer. For women between 35 and 39, 12.7 percent were called back for further tests but only 0.16 percent actually had cancer). – NCI.
Recent NCI data suggests that 29% of women in their 30s undergo mammography which exposes them to many false positive results and unnecessary retesting and biopsies.
Radiation Exposure:
Mammograms initiated at an early age also expose the breast tissue (localized, specific and focused) to increased cumulative lifetime radiation. With a risk of 1 Rad (mSv) causing a 2% (2 in 100)/ year risk would necessarily cause the risk to increase to 20% (2 in 10) in 10 years or 40% (2 in 20) in 20 years of annual mammography. The peak effect from a single intense source of radiation (Hiroshima and Nagasaki data) occurs between 10-15 years, the cumulative effects of annual mammography would account for similar peak/plateau to occur.
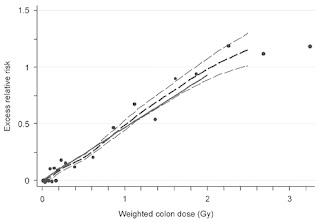
“Tumor registries were initiated in 1957 in Hiroshima and 1958 in Nagasaki. During the period from 1958 to 1998, 7,851 malignancies (first primary) were observed among 44,635 LSS survivors with estimated doses of >0.005 Gy. The excess number of solid cancers is estimated as 848 (10.7%) (Table). The dose-response relationship appears to be linear”
Additional views of the breast to delineate “abnormal” tissues would add to that risk. A known but fortunately rare complication of post radiation therapy following breast-conserving surgery is malignant angiosarcoma. This radiation induced malignancy occurs in elderly individuals with a mean age of 68 years and has an incidence of 0.05-0.2% over a 12.5 year period. Radiation induced angiosarcomas or RIA start as bluish-purple spots on the irradiated breast skin, are detectable by physical examinations and not by mammograms. Median survival in RIA is reported from1.5 to 2.5 years Recurrence rates approach 70 % and 2-year disease free survival ranges from 0–35 % in various series.
NCI (National Cancer Institute) states the following: “Mammograms require very small doses of radiation. The risk of harm from this radiation exposure is low, but repeated x-rays have the potential to cause cancer. The benefits, however, nearly always outweigh the risk..”
Radiation from an X-Ray machine is a low-energy source focused-radiation as is in Computer Tomography scans. (The initial data on CT scans suggests a "probable" risk of cancer in 15,000 amongst 73 million patients who received CT scan procedures).
The energetic from the machine cause dislocation of the electrons within the cells that can disrupt the DNA molecule by changing one of the four Nucleotides: Adenine - Thymine, and Guanine - Cytosine that form the backbone of the DNA helix and the genomic structure. This alteration can lead to disrupted DNA by shutting down a tumor suppressor gene or accelerating a tumor promoter gene or both by changing the down-stream signal transduction into the cell via protein and subsequent cell propagation (growth). These data are not meant to create fearfulness, it merely underscores that persistent continuous exposure is cumulative and methods to mitigate must be considered in future strategies especially for detection.
DNA annealing process
The energetic from the machine cause dislocation of the electrons within the cells that can disrupt the DNA molecule by changing one of the four Nucleotides: Adenine - Thymine, and Guanine - Cytosine that form the backbone of the DNA helix and the genomic structure. This alteration can lead to disrupted DNA by shutting down a tumor suppressor gene or accelerating a tumor promoter gene or both by changing the down-stream signal transduction into the cell via protein and subsequent cell propagation (growth). These data are not meant to create fearfulness, it merely underscores that persistent continuous exposure is cumulative and methods to mitigate must be considered in future strategies especially for detection.
Digital Mammograms:
Digital Mammograms are no different than the Conventional Mammograms except in the mode of recording. The amount of radiation remains the same as does the light source in a digital camera, only the recording method differs; instead of a photographic film, the information is recorded on a CMOS chip. Having said, in digital mammography, due to the ability to modulate contrast, Singh et al. state,“Full-field digital mammography optimizes the lesion-background contrast and gives better sensitivity, and it is possible to see through the dense tissues by altering computer windows; this may be particularly useful in younger women with dense breasts. The need for repeat imaging is reduced, with the added advantage of reduced radiation dose to patients. MRI has a role in screening women at high risk for breast cancer.” This modality also has cost saving benefits built in, since it limits the use of special photographic film; its production, delivery and storage.
Physics of Mammograms:
On an average the human body receives radiation from natural sources, for example the cosmic rays deliver to the tune of 2.4 mSv per year to the human body. Other sources include; the soil that contains various radioactive elements (Potassium 40, Carbon 14 and Radium 226 found in the soil) within and impregnates the foods (Vegetables/fruits) grown in it and transfer the substances into the humans and animals that consume the food. Humans additionally consume the meats from the animals that have consumed the same grown vegetables thus imparting the radioactive elements into the humans again. Fortunately for us humans we have the DNA mismatch repair mechanisms built into us to thwart such daily attacks. It is the cumulation of such events that can over burden the mismatch repair mechanism and diseases then ensue.
Mammograms use low-energy radiation to a total value per test at -20KeV (1 eV or electron volt = 1.602×10^−19 J and 20 KeV = 20 * 1 kiloelectron volt = 20 * 1.60217646 × 10^-16 joules) The absorbed dose is recorded as 0.56% mSv (millisievert (1 mSv = 10^−3 Sv)
The IAEA states, “The biological effects of ionizing radiation vary with the type and energy. A measure of the risk of biological harm is the dose of radiation that the tissues receive. The unit of absorbed radiation dose is the sievert (Sv)”
Increased cancer risk to humans is in 1 in 1000 at 1250 millirem or 8% per Sv (BioPhysics of Radiation)
False Positive:
Taking into account all Mammograms, 9 in 10 abnormal mammograms when subjected to a biopsy are proven negative or said in another way; the yield is 10% (1 in 10) true positivity which means 10% of all abnormal mammograms actually reveal cancer the rest (90%) are proven negative! And speaking of False Negative, which means that the cancer that is present, is not detected by the mammography is an additional conundrum faced by the screening method. Some 10-30% false negative reports are reported. This means that of 1000 women with verified cancer 100-300 will be missed by the diagnostic mammography. This happens due to reader inexperience, oversight, tumor hidden in dense breast or small cancer without telltale signatures. Thus to recapitulate simply: 1 in 10 abnormal mammograms are truly representative of cancer, 2 in 10 mammograms are misread as cancer when there is no evidence of it and 2 in 10 mammograms are misread as normal when cancer exists in the breasts.
Risks and Risk Mitigation:
In younger women the risk of developing breast cancer is dependent upon genetics being the major factor. The family history is extremely important and therefore the directive for extra vigilance. An individual who’s mother or sister with a history of breast cancer especially at a younger age is high risk.
(As are with known BRCA1 and/or BRCA2 gene mutation are considered high risks). BRCA1 and 2 mutation increase the risk by 60% (6 in 10) up to the age of 90 and simultaneously increase the risk of Ovarian cancer by 55% or (55 in100). Thus these younger women at high risk should be subjected to extra vigilance and scrutiny to protect them against the potential diagnosis. Other factors such as menstrual history, breast feeding (protective?), alcohol (lobular breast cancer) radiation therapy, HRT (hormone replacement therapy), and diet/obesity are surrogates of environmental risks and therefore not taken into account for early age related cancer since the damage is limited and risks projected over time.
BRCA gene
(As are with known BRCA1 and/or BRCA2 gene mutation are considered high risks). BRCA1 and 2 mutation increase the risk by 60% (6 in 10) up to the age of 90 and simultaneously increase the risk of Ovarian cancer by 55% or (55 in100). Thus these younger women at high risk should be subjected to extra vigilance and scrutiny to protect them against the potential diagnosis. Other factors such as menstrual history, breast feeding (protective?), alcohol (lobular breast cancer) radiation therapy, HRT (hormone replacement therapy), and diet/obesity are surrogates of environmental risks and therefore not taken into account for early age related cancer since the damage is limited and risks projected over time.
NCI data of risks of breast cancer diagnosis increase with age:
At age 30 the risk is 0.43 in 10 years
At age 40 the risk is 1.45 in 10 years or 1 in 233
At age 50 the risk is 2.38 in 10 years or 1 in 69
At age 60 the risk is 3.45 in 10 years or 1 in 38
At age 70 the risk is 3.74 in 10 years or 1 in 27
At age 80 the risk is 3.02 in 10 years
False Negatives;
So in younger women a family history dictates the need for a diagnostic test. If such a test is needed then a MRI (Magnetic Resonance Imaging) may be the test of choice. Albeit the cost is high but the yield is identical to Mammography! The false negative or missing a diagnosis of cancer, is roughly 20% (2 in 10) with all known testing procedures available today, including the MRI, however the radiation risks are mitigated with the latter.
Feig et al. from Jefferson Medical Center states, “Report of the National Academy of Sciences and a mean breast glandular dose of 4 mGy from a two-view per breast bilateral mammogram, one can estimate that annual mammography of 100,000 women for 10 consecutive years beginning at age 40 will result in at most eight breast cancer deaths during their lifetime. On the other hand, researchers have shown a 24% mortality reduction from biennial screening of women in this age group; this will result in a benefit-to-risk ratio of 48.5 lives saved per life lost.” So although the risks remain, the benefits seem to outweigh in favor for screening women over the age of 40.
Elderly and the Mammogram:
In older women who do not have dense breasts a competent breast examination leads to an extremely high yield of discovery of malignancy 78–83% a close equivalence to mammography. The biologic reason for this is, that in majority of the elderly individuals the disease is more indolent, slow growing and localized. However, screening mammographic examinations yield earlier stage of the disease and therefore potential for curability. In spite of all the screening performed, a recent British Medical Journal Study*(ref) refuted benefits in survival (reduced mortality) amongst women who received mammograms versus those that did not. Further research needs to be done to corroborate this new data.
BI-RADS:
Reporting of Mammograms via the BI-RADS(Breast Imaging Reporting and Database System) method is graded from 0 to 6: 0-2 considered benign. 3, Probably benign, 4 Suspicious, 5 Highly probably cancerous, 6 Malignant
Incidence of Breast Cancer:
The Incidence of late stage Breast Cancer is decreasing both due to diagnostic tests (caused or just discovery?) although a recent downward trend is due to cessation of the HRT and the death rate is also falling due to early diagnosis of DCIS (which carries an excellent 98% 10-year survival) and better management of the disease. The question being, whether the diagnostic testing and disease discovery are just a self-fulfilling prophecy? (Annual mammography, with its inherent radiation effects, over time creates the disease that the test ultimately detects is the plague of thought that pricks the conscience?) More data and research definitely needs to be done to address this issue.
Other Methods of Detection:
Developing non-ionized methods of detection are important for the future. Thermography and Infrared imaging have yet to prove themselves. Unfortunately BSGI (Breast-specific gamma imaging approved recently by the FDA by 23 times) and PEM (Positron Emission Mammography by 20 times more) expose individuals to a higher radiation exposure than mammogram.
MRI as a Diagnostic Tool:
However a portable MRI dedicated for the breast evaluation can easily be developed (One is on the way as you read, this waiting implementation, following more corroborative data). The volume testing would lead to lower costs and limit the annual radiation exposure giving the benefit of 85-87% detection rate currently known and equivalent to mammography. The benefits are that MRI does not lend to cumulative radiation risks.
Medicine is fraught with risks on either side of the diagnostic testing. Too little and the disease runs rampant and too much exposes a patient to unnecessary procedures and the risks mentioned. The straight and narrow path is rarely straight and narrow. Medicine is constantly competing within its own boundaries to help solve the riddle of human disease. It has for millennia from the days of Paracelsus and will into the foreseeable future. In the mean time we seek knowledge to tip the scales in our favor.
References:
Feig S, Hendrick R (1997). "Radiation risk from screening mammography of women aged 40–49 years". J Natl Cancer Inst Monogr (22): 119–24.
Mandelblatt JS, Cronin KA, Bailey S, et al. Effects of mammography screening under different screening schedules: Model estimates of potential benefits and harms. Annals of Internal Medicine 2009; 151(10):738–747
National Cancer Institute: Breast Cancer Screening (PDQ®)―Health Professional. Date last modified 09/03/2010. Available at: http://www.cancer.gov/cancertopics/pdq/screening/breast/HealthProfessional.
Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast cancer screening. New England Journal of Medicine 2005; 353(17):1773–1783.
Singh V, Saunders C, Wylie L, Bourke A., New diagnostic techniques for breast cancer detection. Future Oncol. 2008 Aug;4(4): 501-13.
Miller AB, To T, Baines CJ, et al.. Annual screening with mammography and breast examination did not reduce breast cancer mortality in women 40–49 years of age.
The Canadian National Breast Screening Study-1: breast cancer mortality after 11 to 16 years of follow-up. A randomized screening trial of mammography in women age 40 to 49 years. (2002) Ann Intern Med 137, 305
*Phillipe A, Mathieu B, Anna G, Lars V,. Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ 2011; 343:d4411
Preston DL, Ron E, et al.: Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiation Research 2007; 168:1-64
Givens SS, Ellerbrock NA, et al. Angiosarcoma arising in an irradiated breast. A case review of the literature. Cancer. 1989;64:2214–16.




















No comments:
Post a Comment