Precision Medicine: “An emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person."
Medicine has always been about progress. How to make our lives better, healthier and how we can thwart disease.
Treating patients with some degree of precision has many decades of experience. Although the concept of population medicine was first invoked as similar and only available treatment for most all diseases and blood-letting was it, for any and all disease, understanding real and basic science changed all that. In fact George Washington, the first U.S. president, died after having 3.75 liters of blood removed from his body within a 10 hour period as treatment for a throat infection. Some success in precision medicine goes back to the ABO grouping for blood transfusions. Transfusion reactions are rare nowadays with proper ABO group matching between donor and recipient of the blood.
In 1956 G6PD deficiency was found as the underpinning for favism; toxicity to fave beans and the antimalarial drug primaquine.
As medical research advanced, more interesting phenomena were noted as an impaired CYP2C19 led to Plavix (an anticlotting drug) to become inactive and ineffective. And discovery showed PCSK9 mutation resulted in Lower LDL and consequently people with such mutation had low risk of Cardiovascular Disease. So subsets of humanity with selective gene drivers are making their vulnerabilities and invulnerabilities become known through genomic data.
And that brings me to the…
As medical research advanced, more interesting phenomena were noted as an impaired CYP2C19 led to Plavix (an anticlotting drug) to become inactive and ineffective. And discovery showed PCSK9 mutation resulted in Lower LDL and consequently people with such mutation had low risk of Cardiovascular Disease. So subsets of humanity with selective gene drivers are making their vulnerabilities and invulnerabilities become known through genomic data.
And that brings me to the…
Human Genome Project (HGP), which cost $3 Billion and 13 years of research. At the time the unflinching desire to have HGP cure most human disease was predicted, wrongly. The concept of one gene equals one disease turns out is untrue except in a tiniest of minorities.
Precision Medicine Initiative: Established a $215 millions in 2016 of which $140 million for cohort group (blood, nail, hair samples and follow through) and $75 million for sequencing the genome/administration of the cohort. many successes and an equal amount of misfires will come from this as well.
Intra-tumoral Diversity: Our understanding of the heterogeneity of tumors (cancer cell cluster) shows that a varied number of cancer cells, normal supporting cells, and transitional cells comprise the whole ball of this disaster. Sub-clones within the tumors grow as a Branching Tree adding new genetic mutations as the growth continues. In addition the tumor cell for its own existence is extremely adaptable and therefore plastic.
Multiple cellular pathways with associated Cross talk. Each cell has many different pathways that carry signals from the surface to the core where the engine of division feeds to replicate. Improper signaling can lead to over exuberant growth as in cancer or an arrest of growth and senescence and death of the cell.
Driver Mutation: In cancer there are many mutations that actually drive the cancer growth. Thus far 50 such mutations are known. Some are noted below:
Actionable mutations
i. HER2neu Overexpression of the HER2 protein appeared to occur in approximately 20-25% of breast cancer cases. Herceptin, a drug manufactured against the protein product of the Her 2neu mutation arrests the growth of the cancer. Additionally a newer drug Perjeta is believed to work by targeting a different part of the HER-protein than Herceptin, resulting in further reduction in growth and survival of HER2-positive breast cancer cells.
ii. BRAF V600E: B-Raf mutation on Chromosome 7 drives cell growth via the RAS-RAF-MEK-ERK-MAP Kinase pathway. Vermurafenib a BRAF V600E inhibitor is also a determinant of sensitivity to Proteasome Inhibitor (CARFILZOMIB). 92% BRAF mutation is actually a T(hymine) - A(denine) nucleotide 1796 switch.
iii. BCR-abl mutation Using Imatinib as the drug of choice in CML. Newer refinements of the drugs have managed to enhance the survival of patient afflicted with the chronic myelogenous leukemia.
Dasatinib (Sprycel)
Nilotinib (Tasigna)
Bosutinib (Bosulif)
Ponatinib (Iclusig)
iv. In Lung Cancer EGFR mutation in 50%, Treated with Erlotinib and Geftinib directed against exon 19 deletion, exon 21 L858R, and exon 18 G719X, and Afatinib worked against exon 20 T790M mutation. KRAS mutation in 25% without any specific inhibitors and ALK-EML4 mutation 5-7% of patients with NSCLung Cancer respond well to Crizotinib and Ceritinib.
Passenger Mutation: When certain known driver mutations are located in the part of the DNA that is not proximate to the signaling source, their function is reduced and the risk exposure to the cancer is reduced. BRCA gene is author suppressor gene that overrides any anomalies of organ (breast) cell, therefore mutation that leads to its dysfunction results in cancer:
a. BRCA mutation: BRCA -1 on Chromosome 17 q21.2
Intra-tumoral Diversity: Our understanding of the heterogeneity of tumors (cancer cell cluster) shows that a varied number of cancer cells, normal supporting cells, and transitional cells comprise the whole ball of this disaster. Sub-clones within the tumors grow as a Branching Tree adding new genetic mutations as the growth continues. In addition the tumor cell for its own existence is extremely adaptable and therefore plastic.
Multiple cellular pathways with associated Cross talk. Each cell has many different pathways that carry signals from the surface to the core where the engine of division feeds to replicate. Improper signaling can lead to over exuberant growth as in cancer or an arrest of growth and senescence and death of the cell.
Driver Mutation: In cancer there are many mutations that actually drive the cancer growth. Thus far 50 such mutations are known. Some are noted below:
Actionable mutations
i. HER2neu Overexpression of the HER2 protein appeared to occur in approximately 20-25% of breast cancer cases. Herceptin, a drug manufactured against the protein product of the Her 2neu mutation arrests the growth of the cancer. Additionally a newer drug Perjeta is believed to work by targeting a different part of the HER-protein than Herceptin, resulting in further reduction in growth and survival of HER2-positive breast cancer cells.
ii. BRAF V600E: B-Raf mutation on Chromosome 7 drives cell growth via the RAS-RAF-MEK-ERK-MAP Kinase pathway. Vermurafenib a BRAF V600E inhibitor is also a determinant of sensitivity to Proteasome Inhibitor (CARFILZOMIB). 92% BRAF mutation is actually a T(hymine) - A(denine) nucleotide 1796 switch.
iii. BCR-abl mutation Using Imatinib as the drug of choice in CML. Newer refinements of the drugs have managed to enhance the survival of patient afflicted with the chronic myelogenous leukemia.
Dasatinib (Sprycel)
Nilotinib (Tasigna)
Bosutinib (Bosulif)
Ponatinib (Iclusig)
iv. In Lung Cancer EGFR mutation in 50%, Treated with Erlotinib and Geftinib directed against exon 19 deletion, exon 21 L858R, and exon 18 G719X, and Afatinib worked against exon 20 T790M mutation. KRAS mutation in 25% without any specific inhibitors and ALK-EML4 mutation 5-7% of patients with NSCLung Cancer respond well to Crizotinib and Ceritinib.
Passenger Mutation: When certain known driver mutations are located in the part of the DNA that is not proximate to the signaling source, their function is reduced and the risk exposure to the cancer is reduced. BRCA gene is author suppressor gene that overrides any anomalies of organ (breast) cell, therefore mutation that leads to its dysfunction results in cancer:
a. BRCA mutation: BRCA -1 on Chromosome 17 q21.2
19,581 patients:
46% had Breast Cancer,
12% Ovarian Cancer,
5% Both
37% None
(The effect size is based on the specific location of the mutation. JAMA 4/2015)
c. BRCA-2 on Chromosome13
11,900 patients:
12% Ovarian Cancer,
5% Both
37% None
(The effect size is based on the specific location of the mutation. JAMA 4/2015)
c. BRCA-2 on Chromosome13
11,900 patients:
52% Breast Cancer,
6% Ovarian Cancer,
2% Both,
40% None
c. DiGeorge Syndrome or 22q11.2 deletion syndrome: In this disease, location matters. A slight shift in the placement of this mutation can lead to none of the learning disabilities, congenital heart issues or other disabling anomalies.
d. Cystic Fibrosis: Loss of function mutation as in G551D mutation carrier may not have Cystic Fibrosis but a higher risk of infection…Invacaftor (Kalydeco) helps 4-5% of CF cases.
Not all Mutations are functional (as in location next to the driver gene or further away)or actionable (therapy may be ineffective since the action directed against the wrong gene). JAMA September 2016 article.
Clinical Trials in Precision Medicine (PM):
a. SHIVA Trial: (n=195) No Progression Free Survival or Hazard Ratio differences in genetically matched vs. unmatched.
b. SAFIR-01 Trial: (n=55) 4 Partial Responses and 9 stable disease cases noted in the trial.
c. IMPACT-COMPACT Trial: (n=84) 20% Response Rate in molecular matched vs. 11% in unmatched
d. Basket Trial of 122 patients suggested a BRAF mutation alongside of RAS mutations found in Malignant melanoma, Colorectal and Ovarian Cancers. So the mutations exist not only in selective cancers but these mutations are also shared among other cancers as well. Using Vermurafenib a BRAF V600E inhibitor in these cancer yielded activity.
e. MAP( Molecular Analysis for Personalised Therapy (MAP) conference)Trial: Results from the trial, which took place at the Gustave Roussy Cancer Campus in Paris, found that 199 out of 1110 patients with advanced heavily treated cancer, who had their genes mapped and their treatment tailored, had around 30 per cent longer survival benefit before their cancer started growing again compared to any of the previous therapies the patients had tried. This ranged from between 5 and 32 months.The patients on this trial had diverse types of advanced cancer including lung, breast, head and neck, prostate, bladder, bowel and stomach cancer.
Cost of Precision Drugs
1. As of 2015,150 FDA Approved drugs based on DNA mutations
a. Cystic Fibrosis Drug effective in 5% patients with specific CFTR mutation cost $300,000/year
b. Duchene Muscular Dystrophy: Eteplirsen cost $300,000/ year and recently approved by FDA due to advocacy.
c. A well known debacle in the last decade brought to light a product called Provenge for prostate cancer at a cost of $114,000 that forestalled disease by only 4 months.
These and other costly medications are sticky issues when there are alarm bells sounding on the cost of healthcare. Yet humanity needs to be helped. Reducing administrative and other management costs and redirecting finances to research will auger new advances. As long as a third party insurer dictates the price and governmental policies prevent negotiation of costs, precision medicine may remain a dream for most patients.
Multiple Signal Transduction Pathways.
a. All such treatments based on Biologics have limiting successes. The major one is the plasticity and adaptability of the cancer cells. Cancer cells as normal cells have multiple signaling pathways between the surface and the core and as one is shut down, the cancer cell adapts to create a Cross talk bridge with another pathway to keep the core fed and growing. That is why the response to Biologics are time limited and eventually cancers after an initial regression start to grow. This same mechanism is elicited with resistance to chemotherapy also.
6% Ovarian Cancer,
2% Both,
40% None
c. DiGeorge Syndrome or 22q11.2 deletion syndrome: In this disease, location matters. A slight shift in the placement of this mutation can lead to none of the learning disabilities, congenital heart issues or other disabling anomalies.
d. Cystic Fibrosis: Loss of function mutation as in G551D mutation carrier may not have Cystic Fibrosis but a higher risk of infection…Invacaftor (Kalydeco) helps 4-5% of CF cases.
Not all Mutations are functional (as in location next to the driver gene or further away)or actionable (therapy may be ineffective since the action directed against the wrong gene). JAMA September 2016 article.
Clinical Trials in Precision Medicine (PM):
a. SHIVA Trial: (n=195) No Progression Free Survival or Hazard Ratio differences in genetically matched vs. unmatched.
b. SAFIR-01 Trial: (n=55) 4 Partial Responses and 9 stable disease cases noted in the trial.
c. IMPACT-COMPACT Trial: (n=84) 20% Response Rate in molecular matched vs. 11% in unmatched
d. Basket Trial of 122 patients suggested a BRAF mutation alongside of RAS mutations found in Malignant melanoma, Colorectal and Ovarian Cancers. So the mutations exist not only in selective cancers but these mutations are also shared among other cancers as well. Using Vermurafenib a BRAF V600E inhibitor in these cancer yielded activity.
e. MAP( Molecular Analysis for Personalised Therapy (MAP) conference)Trial: Results from the trial, which took place at the Gustave Roussy Cancer Campus in Paris, found that 199 out of 1110 patients with advanced heavily treated cancer, who had their genes mapped and their treatment tailored, had around 30 per cent longer survival benefit before their cancer started growing again compared to any of the previous therapies the patients had tried. This ranged from between 5 and 32 months.The patients on this trial had diverse types of advanced cancer including lung, breast, head and neck, prostate, bladder, bowel and stomach cancer.
Cost of Precision Drugs
1. As of 2015,150 FDA Approved drugs based on DNA mutations
a. Cystic Fibrosis Drug effective in 5% patients with specific CFTR mutation cost $300,000/year
b. Duchene Muscular Dystrophy: Eteplirsen cost $300,000/ year and recently approved by FDA due to advocacy.
c. A well known debacle in the last decade brought to light a product called Provenge for prostate cancer at a cost of $114,000 that forestalled disease by only 4 months.
These and other costly medications are sticky issues when there are alarm bells sounding on the cost of healthcare. Yet humanity needs to be helped. Reducing administrative and other management costs and redirecting finances to research will auger new advances. As long as a third party insurer dictates the price and governmental policies prevent negotiation of costs, precision medicine may remain a dream for most patients.
Multiple Signal Transduction Pathways.
Example of a single PI3Kinase pathway
a. All such treatments based on Biologics have limiting successes. The major one is the plasticity and adaptability of the cancer cells. Cancer cells as normal cells have multiple signaling pathways between the surface and the core and as one is shut down, the cancer cell adapts to create a Cross talk bridge with another pathway to keep the core fed and growing. That is why the response to Biologics are time limited and eventually cancers after an initial regression start to grow. This same mechanism is elicited with resistance to chemotherapy also.
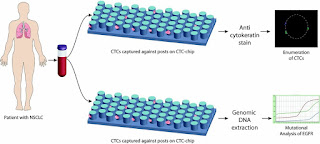
CTCs, Cell Free DNA (cfDNA) and their potential in PM. Although the CTCs and cfDNA have the potential to diagnose and detect abnormal genetic mutations in cancer cells broken free in the blood stream, the problem remains that the mutation noted maybe from part of that branched tree where the cancer has been destroyed but the other branches with ewer mutations might be alive and well. This leads to a conundrum of appropriate therapy as you can surmise.
CTC analyzers
Layered Information: The answer might be in layering information together rather than in piece-meal approaches. One can use the Family history, layer with the genetic mutation, add to that the lifestyle behaviors, which modulate the genome (via an epigenome, as in miRNA) add that to the gut bacterial genome and its impact on the protein production products of said gene modification and there you have a better handle on the disease and its present and future impact. Layering via:
a. Genome
b. Epigenome
c. Microbiome
d. Proteome
NIH in partnership with the FDA and the Biomarkers Consortium embarked on a iSPY 2 Trial where driver mutations in observed sets of patients will be used to treat other sets of patients. this is an attempt to accelerate and advance the process of cancer medicine.