Curious as it might seem, it was. He was a short guy, reminded me of Danny Devito , about four feet nine, with a balding head and thick grey side burns. You would think from his facial profile that he had just emerged from a movie set. His skin was a whiter shade of pale, powdered for effect and the stubble of the five-o-clock shadow stood out in stark relief. He carried a great set of laryngeal chords though. A certain boom in his voice more than made up for his height and pallor.
‘Sir, can you get that for me.” He asked, as I passed by him in the aisle. The “that” was a bottle of 300 pills of Vitamin D3 on the top shelf, much beyond his reach.
“Sure.” I said and gathered the bottle and handed it to him.
“Vitamin D, I see…” I said, hoping to get a response.
But he was not interested in my comments. “Thanks,” he said and pushed his cart in the opposite direction.
It happened again a few months later at a seminar related to over the counter medicines. He was there and after the lecture his voice boomed from the back of the room.
“I have to take issue with you about the Vitamin D.”
The back and forth that followed lasted about fifteen minutes and what was especially interesting was that not a single participant left. Everyone was rooted to the seats, as if spellbound by the dialogue. It turns out our guy is a doctor who had more than a firm conviction in the magical powers of Vitamin D.
Magic or not, there is something to be said about this supplement. Vitamin D has generated a significant amount of literature in the recent past 5-10 years. So, equally the number of proponents have grown with the literature.
Is it magical?
Not really. It is a supplemental vitamin, fat soluble in its characteristics and found abundantly in nature. So what of this recent shine?
Lets look at the basic function first.
Vitamin D functions:
Simply stated the Vitamin D regulates the calcium levels in the blood for both calcific and non-calcific functions. By calcific function, I mean the bones. Vitamin D regulates the calcium homeostasis. The major function at a visible level of calcium is to fill the hollow matrix of collagen tissue of the bones and to render them strong, weight bearing, as armor, as tools for transmission of sound, and as hollow arches and tunnels for transference of air. At the microscopic and invisible level calcium performs admirably in regulating heart function and inter and intra cellular transport networks.
We all know about Rickets, a bone deformity that occurs due to Vitamin D deficiency.
Vitamin D and infection and inflammation:
Looking at the cellular network function we find that Vitamin D is intimately involved with the process of inflammation, and repair of wounds. Its function is to hold the initial repair mechanism to proceed to completion and prevent it from continuing beyond. To understand what that means, consider this: A wound is a breach of tissue. To repair that wound the body brings in an armada of cells that both, put in place a scaffolding to bridge the breach and then remove the dead and effete material (cells) and then put a “coat” of normal layers of skin above the breach so that the trauma appears only as a minor scar. Now suppose that the process of repair continued beyond that, the cellular machinery would be growing cells on top of each other into clumps of tissue that also had admixed within them dead and dying cells and a chaotic growth would follow. One can safely assume this chaotic cellular behavior would create a tumor-like growth following each traumatic breach of the skin or any tissue. A sort of an "unrestrained Keloid” in medical parlance.

Vitamin D has the property of stopping that over-growth. And that is a good thing! Too little would have the opposing effect; delayed healing and infection susceptibility.
Vitamin D and Mortality:
A Chochrane review of 50 randomized controlled trials with 94,000 elderly women showed that Vitamin D3 supplementation reduced all-cause mortality, but most especially supplementing with Vitamin D also reduced the morbidity from vertebral fractures and other skeletal related events with better quality of life. Additionally there is emerging data that deficient individuals also have a higher risk of Type I and II diabetes.
The Cochrane review showed benefits only with Vitamin D3 and not with plain Vitamin D or any of the metabolites taken orally. Of note is that the darker skin (African American blacks) does not allow the UV rays to perform the chemical magic of converting the sterols into Vitamin D3 that is then bound to DBP or Vitamin D binding protein for initiating its functions upon the cells (elicited below).
Consuming more Vitamin D?
Extrapolating on the issues mentioned above, let us look at what would happen if we started chewing on Vitamin D in excess:
The calcium levels would rise dramatically in the blood stream. With the rise of calcium in the blood, more will be excreted via the kidneys through urine leading to stone formation in the urinary tract. That is a painful scenario worth an “ouch.” The high calcium levels would also play havoc with all the organ cellular networks; the heart would suffer cardiac arrhythmia and show on the electrocardiogram initially as prolonged Q-T intervals, the colon would slow down in its motility causing constipation and the brain cells would not be able to maintain their function at higher levels of calcium causing a decay in neural transmission and thus in thought and action.
Vitamin D and Cancer
Now for the good part that we all have been waiting for. What and how does it protect us from cancer?
Fair enough! Vitamin D has been shown to have some beneficial effects against at least four types of cancers; breast, colon, ovary and prostate. Other potential malignancies where it might have the benefit include, osteosarcoma (bone cancer) Glioma (brain tumor) and with “additive” (synergistic) effects to chemotherapy regimens against a whole host of other cancers.
How? How? You say.
Elementary, my dear, elementary!
We are now embarking on a journey into the known. Much remains unknown and therefore subject to reversal in the future. But the path so far traveled is interesting to say the least. To know the bad, we should know the good. To know cancer we have to know the normal physiological and mechanistic functions of the cells. In knowing the normal function any disarray will become obvious as a wayward and ungainly behavior. .
Cells divide for an organism (human, animal most life) to grow. Similarly cells divide in a cancer for it to grow. In that division, there are many stories. We will tackle just a few:
Cell Division and Switches:
For cells to divide they need a “kick-start” that seems to come from a genetic dictate predicated on a physical need, which is, strangely decided upon by a primary genetic calling. Take for instance the male and female germ cells that merge and then the logarithmic division that occurs to create a baby. The cells within the baby grow and then stop and then grow as the needs of the body dictate to keep up with the overall growth. These on-off switches are embedded in our DNA.
Based on the prevailing state of the cell certain genes become over-expressed while others under-expressed. It is the way to control cell function and behavior, almost like having a brake and the accelerator, each applied sequentially as needs arise. There are specific genes that tell cells when they should and should not divide. Remember, I said “switches” well there are a host of known switches and others that we know not of yet.
“Ligand binding causes receptor dimerization and subsequent autophosphorylation of their intracellular tyrosine residues, which in turn phosphorylate other intracellular proteins thereby forming the signal transduction cascade leading to formation of cell cycle regulators which control cell proliferation, differentiation and division. One such signal transduction system involves Ras/ Raf pathway (Ras is a proto-oncogenic product and Raf is a serine/ threonine kinase) which activates the kinase cascade by sequential phosphorylation of the kinases like Raf, Src, MAP (Mitogen-activated protein) and ERK 1/ 2 (Extracellular signal-regulated kinases 1 and 2) leading to gene expression resulting in the progression of the cell cycle and ultimate cell division. It has been observed that constitutive activation of RTK as well as other nonreceptor kinases do occur in many cancers in association with mutations in the genes coding for proteins involved in the kinase cascade.”
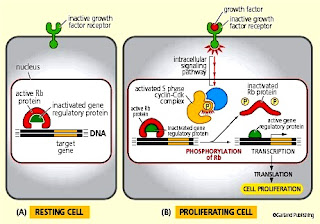
(Translation) The switches cause transmission of signals to travel from the cell surface via receptors, through the cytoplasm of the cell, activating pathways, subsequently riding into the nucleus of the cell where the decision to divide takes place. Mutation of any component of the pathway leads to either an abrogation of the signal or amplification of it –to the detriment of the cell and the organism. If the brakes fail or the accelerator is constantly applied.. you get the message.
What is interesting is that cancer cells as well as normal cells express a surface receptor called the Vitamin D Receptor or VDR (How original!), that binds to a metabolite of Vitamin D called calcitriol “When bound to VDR, calcitriol has been found to regulate the activity of more than 60 genes leading to prodifferentiating, antiproliferative and antimetastatic effects on cells in addition to effects on cell cycle and angiogenesis (antiangiogenic).” In other words calcitriol shuts down the proliferative (growing ability) of the cell to multiply/divide and spread..
One comprehensive gene product that keeps cells in check is the Rb gene. This gene has to remain in a hypo(low)phosphorylated state (inactive) Vitamin D (calcitriol) keeps it so. Rb gene in a hypo(low)phosphorylated state, binds with the E2F transcription factors and arrests the cell cycle growth phase.
In cancers of the breast, prostate, colon and ovaries calcitriol is known to dephosphorylate the Rb gene product leading to a blockade of cancer cells at a checkpoint-1 in the cell cycle. Conversely Phosphorylation of the Rb gene has the opposite effect and leads to unchecked cell growth. Speaking about the cell cycle, one is reminded of an oxen-driven water well. Consider the owner as the p53 gene (p53 another very important gene is considered as the Guardian of the Genome”), the oxen as the power source, the mechanical brake as the Caspase system and the cans of water on the metal wire containing the new dividing cells.

The p53 gene/protein product determines when the oxen start and stop. The Oxen (hormones, protein and the process of phosphorylation) have to be fed to work and the cans bring up the water (newly divided cells). If brackish water comes up in the cans, the owner investigates the well and either applies a brake, puts a filter or digs the well deeper to get to the newer water stratum for cleaner supply. So in this thought process, onsider Vitamin D as one of the brake/filter in the oxen driven well water system.
This downregulation of the various pathways is inherent to the Vitamin D byproducts such as calcitriol that mates with the VDRs to induce a “downstream” signal to the center of the aberrant (cancer) cell nucleus and tells it to stop growing. In other words, Vitamin D “may” bring(s) sanity to potential chaos.
Another mechanism used by Vitamin D (known via basic hard science) is creating an over expression of a protein called cystatin-D:
“Cystatin-D is antitumorigenic and antimetastatic. It inhibits these endogenous cysteine proteases (endosomal/ lysosomal), has some modulatory role in cell proliferation, differentiation, survival and migration in addition to interleukin and nitric oxide production. It also inhibits migration and anchorage - independent growth, antagonizes Wnt/β-catenin signaling pathway (Wnt is an oncogene which codes for the growth factor Wnt), represses c-myc and expression of a number of epithelial-mesenchymal transition inducers (SNAI1, SNAI2, ZEB1 and ZEB2) which are involved in the progression of primary tumors towards metastasis. The protein (cystatin D) induces E-cadherin expression which is repressed during epithelial-mesenchymal transition period.”
(Translation) Cystatin-D prevents cellular differentiation and migration of the cell and inhibits certain key genetic promoters to cause a phase-transition, eg EMT (Epithelial-Mesenchymal Transition). EMT is known to occur in malignancies allowing cells to co-opt normal cells to allow tunneling and escape into the open.
Additionally Cystatin-D also (upregulates ) jazzes up the BAX system (that promotes bad cell apoptosis/death) and (downregulates) mutes the BCL2 system (that prevents cell apoptosis/death). This inverse underpinning keeps the bad/cancer cell growth from achieving out of control proliferative state. This mechanism has been contemplated to help reduce the risk of Non Hodgkin Lymphoma.
Interestingly Calcitriol also has some of these “magical” properties of enhancing the VDR on the cell surface for increased binding and thus increased influence on cellular behavior (One might consider the role of the lobbyists in determining policy in Washington).
Before you go running to your garage and speeding in your car to the local drug store, let me mention a few caveats: The determination of these mechanistic actions have been seen in-vitro studies (in the Petri dish in the labs, that is) Large scale studies in humans have been done using retrospective (looking backwards into the past) epidemiological and case controlled studies. There is a wide gulf between the “this” and the “that.” The correlative forces between what has been seen in human studies seem likely to be compliant with the lab studies for they seem to confirm the mechanism underlying the overall findings, yet a word of caution here it seems is prudent: In a multivariate system a univariate determination for causation is fraught with pot holes. The bird eye view looking down on the entire premise is virtuous. We are beginning to peer down into this microscopic cellular fiefdom and it has some strange stories to tell.
So allow me to throw a cautionary tale in here: Vitamin D3 inside the body can also be co-opted by the cancer cell to convert its signal from one enforcing “proapoptosis” or forcing death of bad cell into an “antiapoptotic” signal as Duque et al suggest in their 2004 paper:
“Perhaps the most significant finding is that mutp53 can convert vitamin D3 from a proapoptotic agent into an antiapoptotic one. In support of this notion, vitamin D3 suppresses death receptor-mediated apoptosis in OVCAR3 ovarian carcinoma cells (Zhang et al., 2005b), which harbor endogenous mutp53. Conceivably, some cancers might have evolved a mechanism that allows them to capitalize more efficiently on the survival route of VDR while evading its proapoptotic effects. Our data suggests that acquisition of gain-of-function p53 mutations may constitute one such mechanism. Obviously, p53 mutations alone are not sufficient to drive the conversion of the VDR pathway into an antiapoptotic one, as not all mutp53-expressing tumor-derived cell lines are equally protected by vitamin D3. Thus, additional alterations most likely cooperate with mutp53 to orchestrate the antiapoptotic response to vitamin D3. Identification of such cooperating factors remains an important challenge. However, in addition to the well documented proapoptotic effects, there are circumstances where vitamin D3 exerts antiapoptotic effects, including increased cell survival following UV trauma and protection of some cancer cell lines from killing by cytotoxic drugs. An inhibitory effect of vitamin D3 on TNFα-induced apoptosis and on TRAIL and Fas ligand-induced apoptosis, accompanied by a decrease in Bax and upregulation of Bcl2 and p21, has also been described.” Translation: Vitamin D3 can be co-opted by a mutated p53 into doing exactly the opposite of what it does in normal circumstance. So different scenarios may breed different results. Thus high levels may actually in an underlying mutated gene scenario create a monster that we have been trying to avoid facing. That is why being extra caution is indeed the right way to proceed, lest we broadcast the wrong message to everyone.
Vitamin D and individual Cancers:
Breast Cancer:
Vitamin D and Breast Cancer studies have revealed several interesting features. The most recent one presented at the San Antonio Breast Conference in December 2011, Hates, et.al. showed in a retrospective analysis that the size of the initial presentation of the breast cancer was inversely associated with the level of the Vitamin D in the blood. The correlation was significant to a high degree level at p-value=0.0063.
“In a retrospective study, lower vitamin D levels were significantly associated with larger tumor size (P=0.0063), Barbara Brouwers, PhD, of the University of Leuven in Belgium, reported during a poster session at the San Antonio Breast Cancer Symposium.”
Looking back at other studies there are other associative features, including the risk reduction between high levels of Vitamin D and lower risk of Estrogen Receptor Positive and negative breast cancer models (Jin Lee Hong et al.).
“In conclusion, we investigated the in vivo effect of certain Gemini vitamin D analogs on mammary tumor growth in a chemically-induced breast cancer model and in a xenograft model. We report here that Gemini vitamin D analogs significantly inhibit both ER-positive and ER-negative mammary tumor growth without increasing serum calcium levels. Mechanistic studies showed that the inhibitory activity was associated with the induction of IGFBP-3 and the CDK inhibitor p21 in both animal models.”
Using age as a defining criterion, the postmenopausal breast cancer patients who had a high level of Vitamin D level also had a lower risk of aggressive disease. (Robien et al) These data suggest some degree of correlation between the cancer of the breast and some modulating features of Vitamin D. One of the etiologies of this suppressive pressure seems to be the anti-inflammatory effect of the disease through the induction of the NFkB (Nuclear Factor kappa B), which is intimately involved with inflammation and may be the driving force as a promoter of the disease in malignancies. More data will have to be gathered for confirmation. The authors caution: “Changes in vitamin D intake over time might have contributed to the diminished association observed in later years” The word “May” stands out in stark contrast, doesn’t it? We seem to be looking for answers and finding them. “Seek and ye shall find!”
Prostate Cancer:
Kovlenko et al show the importance of VDR in prostate cell growth and the risks of procancerogenic events related to low VDR either to lower dietary intake or subsequent deletion by other factors. While this data is suggestive of the promissory intent of the VDR, it is at best a correlation. Similarly Yang et al, found; “that inhibition of Snail-1 signaling by transfection could increase the expression of VDR, enhance the anti-proliferative activity of 1,25(OH)-D(3) in osteosarcoma cells, and induce apoptosis and lower invasion in vitro.
Therefore, strategies to suppress Snail-mediated signaling may lead to the better action of 1,25(OH)-D(3) as an anti osteosarcoma treatment.”
Melanoma:
In Melanoma cell lines the Vitamin D3 acts protective against cancer via the fas-mediated pro-apoptotic pathway via the immunogenic Natural Killer (NK) cells. However moderate to sever exposure to the sun in people who have a preexisting history of at least one skin melanoma show an association with VDR gene polymorphism (Bsml). In other words there appears to be an underlying damaged gene that transposes the risk for future occurrences by making Vitamin D ineffective due to the inherent VDR (polymorphism) mutation. (Mocellin et al and Mendelcorn-Monson et al) What that means simply is that even Vitamin D polymorphism (mutation) make the function of Vitamin D in protecting health moot. However this is a relatively infrequent occurrence.
(Translation) A messed up VDR by virtue of a messed up gene makes Vitamin D therapy ineffective.
Bone Metastasis:
As mentioned previously, since Vitamin D plays a major role in the homeostasis of calcium and the maintenance of normal bone structure and remodeling, it has been shown that deficiency of Vitamin D leads to growth of metastases from prostate cancer into the bone. Zheng et al suggest through experimentation: “At endpoint, osteolytic and osteosclerotic lesion areas, total tumor area, and tumor mitotic activity were all significantly increased in vitamin D deficient mice compared to controls. Vitamin D deficiency stimulates prostate cancer growth in bone through modulating the bone microenvironment.”
Translation not needed. This might be as a result of the structural porosity caused by the low calcium level and lack of protection of pathway inhibition by the low levels of Vitamin D.
While on the subject of Prostate Cancer another study shows a direct relation between VDR expression, Vitamin D and a reduced risk of progression, reiterating the finding that the VDR when joined with the Vitamin D promote cellular restraint and slow down the rate of progression of disease. Prospective studies need to be done to confirm the VDR levels, Vitamin D3 levels and the rate of spread of Prostate Cancer for further proof.
Colon Cancer:
In Colon Cancer Davis et al suggest: “A wealth of scientific evidence supports a role for vitamin D in decreasing colorectal cancer incidence, and possibly mortality. This reduction in risk is related to inhibition of cellular proliferation and stimulation of differentiation”
Remember the Wnt pathway, I mentioned earlier in this discourse and its relation to VDR and Vitamin D. Well here it is again. Apparently there is some control of the Wnt pathway inhibition exercised by the VDR and calcium. The result is that B-Catenin does not accumulate in the nucleus to send a message to the genes to become active and tell the cell to grow. However if this allowed to proceed, then B-Catenin binds to TCF4 that activates another gene product “myc” that allows entry into the nucleus promoting the cancer cell through cell cycle advance and division.
“Binding of WNT to FZ activates one of two pathways: the canonical pathway, which involves β-catenin and controls cellular proliferation; and the planar pathway, which involves Ca2+ and is important in cellular movement and polarity. Briefly, in the canonical pathway, in the absence of WNT, cytosolic β-catenin, which is normally bound to membranous E-cadherin, interacts with the 'destruction complex', which is composed of the tumor-suppressor protein APC (adenomatous polyposis coli), glycogen synthase kinase 3β and axin. This results in serine phosphorylation of β-catenin, its recognition by an E3 ubiquitin ligase, and its degradation. If, however, WNT is present it binds to FZ, the kinase activity of the destruction complex is blocked, and β-catenin remains unphosphorylated, resulting in accumulation of β-catenin in the nucleus. This enables β-catenin to bind to the transcription factor TCF4 that can activate downstream target genes such as the proto-oncogene MYC that promotes entry of the cell into the S-phase of the cell cycle. The small intestine of mice lacking a functional Tcf4 gene is populated only by cell-cycle-arrested, differentiated epithelial cells, the nuclei of which have accumulated β-catenin.”
Non-Hodgkin Lymphoma:
Now before your eyes cross and your teeth chatter, let me also mention that Vitamin D seems to have a protective effect on Non Hodgkins Lymphoma. This data is garnered from epidemiology studies only and subject to criticism. However what is not prone to ridicule is the fact that Vitamin D3 potentiates the effects of chemotherapeutic agents such as Gemcytabine and Cisplatin when used in bladder cancer cell models in vitro (lab) and in vivo (in animal models). These studies presage the next experimental protocols utilizing studies in humans for corroboration.
I find it important to mention the strong language used by Ma et al in his support for Vitamin D and its protective effects: “Calcitriol elicits anti-tumor effects mainly through the induction of cancer cell apoptosis, cell cycle arrest, differentiation, angiogenesis and the inhibition of cell invasiveness by a number of mechanisms. Calcitriol enhances the cytotoxic effects of gamma irradiation and certain antioxidants and naturally derived compounds. Inhibition of calcitriol metabolism by 24-hydroxylase promotes growth inhibition effect of calcitriol. Calcitriol has been used in a number of clinical trials and it is important to note that sufficient dose and exposure to calcitriol is critical to achieve anti-tumor effect.”
Vitamin D Testing:
Vitamin D testing has come under a lot of scrutiny. Since methodologies differ and the exact needs of an individual person remain unknown, people have extrapolated the blood levels empirically. Real hard facts remain still enshrouded in mystery, although we are peeling the onion layers diligently. The bare facts about its mechanism are fairly well known: “The Vitamin D is called a "vitamin" because of its availability from an exogenous source, predominately from oily fish in the form of cholecalciferol, vitamin D3. Plant-based vitamin D is in the form of ergocalciferol, D2.It is really a hormone, as it is synthesized by the skin and metabolized by the liver and then, the kidney to an active hormone, calcitriol, which then acts in its classical action to absorb calcium from the intestine, and promote bone mineralization. In the skin, 7-dehydrocholesterol is converted to vitamin D3 in response to sunlight, a process that is inhibited by sunscreen with a skin protection factor (SPF) of 8 or greater. Once in the blood, vitamin D2 or D3 from diet, or D3 from skin production are carried by an alpha-2-globulin, vitamin D binding protein, and are carried to the liver where they are hydroxylated to yield 25-hydroxyvitamin D (25OHD; calcidiol). 25OHD then is converted in the kidney to 1, 25(OH)2D (calcitriol) by the action of 25OHD-1-alpha hydroxylase (CYP27B1). The CYP27B1 in the kidney is regulated by nearly every hormone involved in calcium homeostasis, and its activity is stimulated by PTH, estrogen, calcitonin, prolactin, growth hormone, low calcium levels, and low phosphorus levels. Its activity is inhibited by calcitriol, thus providing the feedback loop that helps regulates its synthesis.”
Heart Disease:
Q: So what is the ideal level of Vitamin D in the blood?
A: Some profess 50 nMol/ml. Others are not sure. The problem is that the value is extrapolated from data gathered via epidemiological studies. A prospective large cohort study has yet to be undertaken. The dilemma of recommending the real dosage and trying to achieve the “real right level” in the blood is difficult.
Q: Is more Vitamin D intake safe?
A: No! absolutely not, as previously articulated.
Q: Is a Vitamin D deficiency a potential source of bad health?
A: Seems so, based on the previous discussion.
Q: Does the right amount prevent against various cancers?
A: Strongly suspected but not confirmed.
Q: Does the right level of Vitamin D protect against heart disease?
A: Yes it seems so! Vacek et al conclude from their single institution study spread over 5 years and 8 months They use the cutoff value at 30 nMol/ml: “Vitamin D deficiency was associated with several cardiovascular-related diseases, including hypertension, coronary artery disease, cardiomyopathy, and diabetes (all p <0.05). Vitamin D deficiency was a strong independent predictor of all-cause death (odds ratios 2.64, 95% confidence interval 1.901 to 3.662, p <0.0001) after adjusting for multiple clinical variables. Vitamin D supplementation conferred substantial survival benefit (odds ratio for death 0.39, 95% confidence interval 0.277 to 0.534, p <0.0001). In conclusion, vitamin D deficiency was associated with a significant risk of cardiovascular disease and reduced survival. Vitamin D supplementation was significantly associated with better survival, specifically in patients with documented deficiency.”
Mechanism of action in Heart Disease:
Although the mechanism of action in the relationship between heart disease and Vitamin D deficiency remains elusive, preliminary data seem to show that it causes inhibition of cardiomyoblasts (primitive heart cells) growth, reduces inflammation (considered a precursor to coronary disease) expresses the production of cardiomyotubes which direct nutrients to the cells and stabilizes the cardiac cells themselves.
And so, you don’t get too comfortable in your pajamas reading this, guess what? One of the hallmarks of testing for heart disease event risk is the “calcification” found in the coronary arteries. The issue then arises; does the calcification occur because of too much calcium (related to Vitamin D?) in the blood (metastatic) or due to preceding damage with atherosclerosis of the blood vessels, caused as a result of inflammation and calcium deposition is secondary (dystrophic). You see the “head-scratching” that goes on in real science! Answer still eludes us. In fact recent data in another meta analysis failed to show any benefits in heart disease or cancer. So there!
This discourse is a nonlinear multi-directional attempt at relegating, the mysteries of Vitamin D and its many nuances in the life of a living cell, to knowledge. Its effects on humans translated axiomatically via basic science. Prospective studies have yet to show the benefits proposed and thus are eagerly sought. Human epidemiological studies are fraught with risks in correlating assumptions with causations and thus the warnings and disclaimers. What the epidemiological studies do is, set the stage for confirmatory data. The problem is often in the eye of the beholder. The experimentalist who sets out to prove the epidemiological data will most likely, through his “rose-colored glasses” find identity with the preceding study. Unless, that information is vouched for by basic experimental science, shards of untruths maybe in store to prick the balloon of gathered information.
There are many rungs to this ladder. We have just stepped on the very first rung. What we may find on the next one and the one after is something new that may change our entire viewpoint, or confirm without a shred of doubt the premise we seek to annul or uphold. For truth in real science is to shed individual and prevalent bias and arrive at an understanding.
Where can we find Vitamin D? You ask. Oh it is everywhere. Go outdoors and bask in the sun each day and your body will produce enough of it to keep your levels within norm. And Oh by the way, spending the entire day under fluorescent lights and then running off to the beach to get cooked is damaging to the skin. Moderation is called for as in all other aspects of life. But if you must live in the glare of the computer screen under artificial life eating bonbons then there are Vitamin D pills available.
I wonder how the pale-faced doctor with the grey sideburns we met earlier, is holding up? An outdoor walk might help. Don’t you think?
Summary:
- Vitamin D is involved with the Homeostasis of Calcium in the bones and soft tissues
- Cells express VDR or Vitamin D Receptors that merge with Vitamin D to signal into the cell.
- Byproduct of Vitamin D promotes more VDR as need arises.
- Once the VDR merges with Vitamin D the signal goes through the cytoplasm of the cell into the nucleus to cease extravagant proliferation.
- Cancers use various pathways to bypass the growth restraints. Vitamin D seems to reaffirm those restraints.
- Studies suggest Vitamin D protects the heart in some manner the exact mechanism still remains unknown.
- Vitamin D testing and actual threshold value of protection remains elusive.
- We can all get plenty of Vitamin D by frequently taking a walk in the sun.
A man only becomes wise when he begins to calculate the approximate depth of his ignorance.
~Gian Carlo Menotti
References:
Chiang KC, Yeh CN, Chen HY, Lee JM, Juang HH, Chen MF, Takano M, Kittaka A, Chen TC..
19-Nor-2α-(3-hydroxypropyl)-1α,25-dihydroxyvitamin D(3) (MART-10) is a potent cell growth regulator with enhanced chemotherapeutic potency in liver cancer cells. Steroids. 2011 Dec 11;76(13):1513-9. Epub 2011 Aug 25
Kovalenko PL, Zhang Z, Yu JG, Li Y, Clinton SK, Fleet JC..
Dietary vitamin d and vitamin d receptor level modulate epithelial cell proliferation and apoptosis in the prostate. Cancer Prev Res (Phila). 2011 Oct;4(10):1617-25. Epub 2011 Aug 11
Bjelakovic G, Gluud LL, Nikolova D, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev. Jul 6 2011
Bischoff-Ferrari HA, Willett WC, Wong JB, et al. Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med. Mar 23 2009;169(6):551-61
Joergensen C, Hovind P, Schmedes A, Parving HH, Rossing P. Vitamin d levels, microvascular complications, and mortality in type 1 diabetes. Diabetes Care. May 2011;34(5):1081-5.
Yang H, Zhang Y, Zhou Z, Jiang X, Shen A..
Snail-1 regulates VDR signaling and inhibits 1,25(OH)-D(3) action in osteosarcoma.. Eur J Pharmacol. 2011 Sep 22
Lee JH, Park S, Cheon S, Lee JH, Kim S, Hur DY, Kim TS, Yoon SR, Yang Y, Bang SI, Park H, Lee HT, Cho D..
1,25-Dihydroxyvitamin D(3) enhances NK susceptibility of human melanoma cells via Hsp60-mediated FAS expression. Eur J Immunol. 2011 Oct;41(10):2937-46. doi: 10.1002/eji.201141597. Epub 2011 Sep 6
Bao BY, Yao J, Lee YF. 1alpha, 25-dihydroxyvitamin D3 suppresses interleukin-8-mediated prostate
cancer cell angiogenesis. Carcinogenesis 2006;27:1883-93.
Bernardi RJ, Johnson CS, Modzelewski RA, Trump DL. Antiproliferative effects of 1alpha,25- dihydroxyvitamin D(3) and vitamin D analogs on tumor-derived endothelial cells. Endocrinology
2002;143:2508-14.
Maruyama R, Toyota M, Suzuki H, Sasaki Y, Aoki F, Shinomura Y, et al. The functional relation of vitamin D receptor and p53 in cancer ce Prevention Research; Nov. 12-15, 2006.
Cross HS, Hulla W, Tong W, Peterlik M. Growth regulation of human colon adenocarcinoma-derived cells by calcium, vitamin D and epidermal growth factor. J Nutr 1995;125:2004-8.
Chiang KC, Yeh CN, Chen MF, Chen TC.
Hepatoceclullar Carcinoma and Vitamin D- A review.. J Gastroenterol Hepatol. 2011 Aug 22.
Vanoirbeek E, Krishnan A, Eelen G, Verlinden L, Bouillon R, Feldman D, Verstuyf A..
The anti-cancer and anti-inflammatory actions of 1,25(OH)2D3. Best Pract Res Clin Endocrinol Metab. 2011 Aug;25(4):593-604
Robien K,
Cutler GJ,
Lazovich D. Vitamin D intake and breast cancer risk in postmenopausal women: the Iowa Women's Health Study.
Cancer Causes Control. 2007 Sep;18(7):775-82. Epub 2007 Jun 5.
Hatse S, et al "Vitamin D status in newly diagnosed breast cancer patients inversely correlates with tumor size and moderately correlates with outcome" SABCS 2011; Abstract P5-05-01.
Hong Jin Lee, et al. Gemini Vitamin D Analogs Inhibit Estrogen Receptor Positive and Estrogen Receptor Negative Mammary Tumorigenesis without Hypercalcemic Toxicity.
Cancer Prev Res (Phila). 2008 November; 1(6): 476–484.
Mocellin S, Nitti D..
Vitamin D receptor polymorphisms and the risk of cutaneous melanoma: a systematic review and meta-analysis. Cancer. 2008 Nov 1;113(9):2398-407. Review
Mandelcorn-Monson R, Marrett L, Kricker A, Armstrong BK, Orlow I, Goumas C, Paine S, Rosso S, Thomas N, Millikan RC, Pole JD, Cotignola J, Rosen C, Kanetsky PA, Lee-Taylor J, Begg CB, Berwick M.
Sun exposure, vitamin D receptor polymorphisms FokI and BsmI and risk of multiple primary melanoma. Cancer Epidemiol. 2011 May 23.
Gustavo Duque, Khadija El Abdaimi
a, Janet E Henderson
c, Abderrahim Lomri
d, Richard KremerVitamin D inhibits Fas ligand-induced apoptosis in human osteoblasts by regulating components of both the mitochondrial and Fas-related pathways.
Bone Volume 35, Issue 1, July 2004, Pages 57-64
Zheng Y, Zhou H, Ooi LL, Snir AD, Dunstan CR, Seibel MJ..
Vitamin D deficiency promotes prostate cancer growth in bone. Prostate. 2011 Jun 15;71(9):1012-21
Hendrickson WK, Flavin R, Kasperzyk JL, Fiorentino M, Fang F, Lis R, Fiore C, Penney KL, Ma J, Kantoff PW, Stampfer MJ, Loda M, Mucci LA, Giovannucci E..
Vitamin D receptor protein expression in tumor tissue and prostate cancer progression. J Clin Oncol. 2011 Jun 10;29(17):2378-85
Davis CD, Milner JA..
Vitamin D and colon cancer. Expert Rev Gastroenterol Hepatol. 2011 Feb;5(1):67-81. Review
Plvarez-Díaz S, Valle N, García JM, Peña C, Freije JMP, Quesada V, et al. Cystatin D is a candidate tumor suppressor gene induced by vitamin D in human colon cancer cells. J Clin Invest 2009;119:2343-58.
Ma Y, Trump DL, Johnson CS..
Vitamin D in combination cancer treatment. J Cancer. 2010 Jul 15;1:101-7
Kaler P, Galea V, Augenlicht L, Klampfer L..
Tumor associated macrophages protect colon cancer cells from TRAIL-induced apoptosis through IL-1beta-dependent stabilization of Snail in tumor cells.
PLoS One. 2010 Jul 22;5(7)
Ma Y, Yu WD, Trump DL, Johnson CS..
1,25D3 enhances antitumor activity of gemcitabine and cisplatin in human bladder cancer models. Cancer. 2010 Jul 1;116(13):3294-303
Stambolsky P, Tabach Y, Fontemaggi G, Weisz L, Maor-Aloni R, Siegfried Z, Shiff I, Kogan I, Shay M, Kalo E, Blandino G, Simon I, Oren M, Rotter V..
Modulation of the vitamin D3 response by cancer-associated mutant p53. Cancer Cell. 2010 Mar 16;17(3):273-85. Erratum in: Cancer Cell. 2010 May 18;17(5):523.
Kelly JL, Friedberg JW, Calvi LM, van Wijngaarden E, Fisher SG..
Vitamin D and non-Hodgkin lymphoma risk in adults: a review. Cancer Invest. 2009 Nov;27(9):942-51. Review
Reya T and Clevers H (2005) Wnt signalling in stem cells and cancer. Nature 434: 843-850
Mao B et al. (2001) LDL-receptor-related protein 6 is a receptor for Dickkopf proteins. Nature 411: 321-325
Kohn AD and Moon RT (2005) Wnt and calcium signaling: β-catenin-independent pathways. Cell Calcium 38: 439-446
He TC et al. (1998) Identification of c-MYC as a target of the APC pathway. Science 281: 1509-1512
Korinek V et al. (1998) Depletion of epithelial stem-cell compartments in the small intestine of mice lacking Tcf-4. Nat Genet 19: 379-383
Vacek JL,
Vanga SR,
Good M,
Lai SM,
Lakkireddy D,
Howard PA.. Vitamin D Deficiency and Supplementation and Relation to Cardiovascular Health.
Am J Cardiol. 2011 Nov 7.
http://jcem.endojournals.org/content/early/2011/11/17/jc.2011-1309